PET scans and contrast enhanced magnetic resonance imaging (MRI) have improved lesion detection but definitive diagnosis and/or molecular profiling still requires biopsy specimens. These procedures are performed with ultrasound and computed tomography guidance. The challenge of targeting a lesion visible on imaging technologies not available in the procedure room is resolved with the use of navigation technologies. Using fusion, images from pre-procedural modalities can be registered to intra-procedural ultrasound, CT or even CBCT enabling advancement of a needle or an ablation probe to the lesion.
Publications by the UCI IR physicians have shown that these technologies allow targeting lesions not visible on conventional imaging and/or targeting specific area in a lesion such as guiding a biopsy needle into the PET avid area or the non-necrotic portion of a lesion. A prospective randomized trial by Dr Abi-Jaoudeh comparing navigation technologies to conventional imaging for lesions seen on ultrasound or CT demonstrated that use of these technologies reduced the time and the number of needle repositioning required to reach a target. Needle repositioning are associated with increased risk of complications and, therefore, this technology improves patient safety.
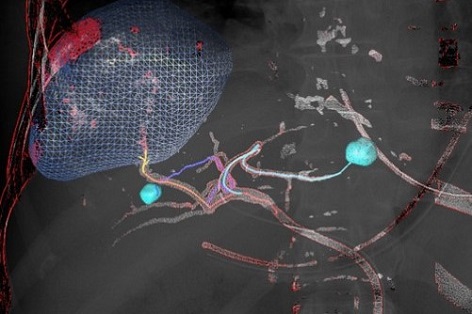
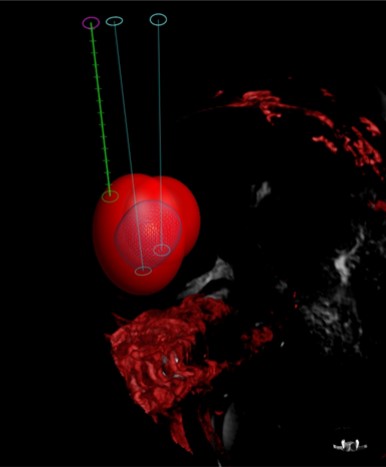
These image fusion techniques can be used to plan ablation and embolization procedures. The tumor can be segmented on advanced intra-procedural imaging, the ablation probe trajectories can be planned in advance and displayed in real time. The predicated ablation zone can be displayed to ensure coverage of the tumor with a safety margin. Finally, once completed the ablation zone is segmented to confirm complete treatment coverage of the tumor. The use of image fusion and navigation technologies resulted in changes in number of ablation probes and/ or duration of ablation in 1/3 of patients with technical effectiveness at one month of 96.1%.
During embolization, these technologies have been shown to improve detection of the number of vessels supplying a tumor that need to be treated. The post embolization scans can be overlaid to the pre-treatment scan to ensure that the entire tumor has been treated. Complete tumor coverage by embolization has been shown to increase the rate of complete response and progression free survival in patients with hepatocellular carcinoma. Therefore, use of these advanced imaging technologies is correlated with improved patient outcome.
Another potential advantage of these technologies is possibility of reduction in contrast use and radiation. Indeed, in the prospective biopsy trial, the skin entry radiation dose decreased by 29%. Also, there was a 50mL reduction in contrast use compared to conventional imaging.
Nadine Abi-Jaoudeh, MD

